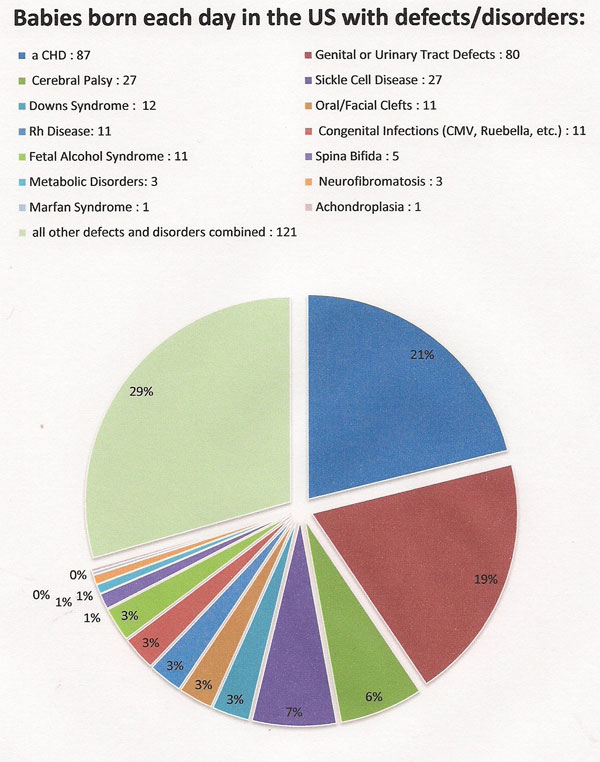
Congenital heart defects are responsible for more deaths in the first year of life than any other birth defects, the National Institutes of Health reports.
Need for Awareness - Research:
For every dollar provided by the national medical funding arm of the American government, the National Institute of Health (NIH), only one penny is provided for pediatric research, and only a portion of that penny goes to support research on heart defects, the most common birth defect. (Children's Heart Foundation)
Statistics:
According to the United Network of Organ Sharing (UNOS) in 1997, there were 277 hearts transplanted in children between 0 and 17 years of age.
In 1998, 707 children from 0-17 were listed with UNOS for a heart transplant.
In 1998, 265 heart transplants were performed.
Meaning that 442 children aged 0-17 died while waiting for a heart transplant and 884 moms and dads said good-bye to their child.
In 2006 Phoenix was one of those children.
Clearly there is a need to raise awareness of the need for organ donation.
There are an estimated 180,000 adults living with heart defects in Canada right now. Approximately 38,000 adults and 30,000 children in Ontario have a heart defect. Ontario has the highest rate of births with heart defects in Canada.
1 in 70 Canadian newborns are affected by a heart defect.
Hypoplastic Left Heart syndrome (HLHS) : HLHS is the condition that Phoenix was born with and he passed away from complications of it.
Hypoplastic left heart syndrome, or HLHS for short, means that the left side of the heart did not develop normally. Therefore, the mitral and aortic valves are usually tiny or absent, as are the the left ventricle and the first part of the aorta. Perhaps the most critical defect in HLHS is the small, underdeveloped left ventricle. In a normal heart, this chamber is very strong and muscular so it can pump blood to the body. When the chamber is small and poorly developed, it will not function effectively and cannot provide enough blood flow to meet the body's needs. For this reason, an infant with HLHS will not live long without surgical intervention. Parents are given a number of options depending on when the diagnosis is made potentially including - abortion of the fetus, compassionate care (no surgical intervention which results in the baby passing away usually within the first two weeks of life) or one of a number of surgical option.
There are two, possibly three, surgical options; one is cardiac transplantation, in which the heart is replaced by a donated heart, another is a 3-staged surgical procedure and the last surgical option is only available for a subset of HLHS patients and is called a biventricular repair.
The three-step procedure is called "the Norwood" because the first operation is called the Norwood Procedure. The Norwood is done very soon after birth, usually within the first few days of life. The second step is called the hemi-Fontan (which is frequently a bi-directional Glenn operation). It sends half of the blood returning from the body to the lungs, reducing the workload on the heart. This second step is part of the preparation to transform the HLHS heart into a two-chamber pumping heart which will only function to pump blood to the body (after the third operation, all of the blood will travel passively to the lungs). The third operation is called the Fontan operation. In this operation, the other half of the blood returning from the body to the heart is sent instead to the lungs. In what used to be a uniformly fatal disease, consider the following statistics from the very best facilities treating HLHS:
- Survival following a Norwood operation is around 80%
- Survival following a bi-directional Glenn operation is around 100%
- Survival following a Fontan operation is around 95%
- Overall, survival at 5 years of age is around 70 - 75%
These statistics are not representative of EVERY facility treating HLHS, so it is imperative parents ask their children's doctors for information BEFORE a treatment facility is chosen - if there is time. This is one of the advantages of finding out about the HLHS diagnosis in utero.
Most patients who get through the three stages do quite well. They are able to lead a fairly normal life with few restrictions. Most patients have to be on some kind of anticoagulant (like baby aspirin), many need Digoxin, some kind of diuretic (at least for some time post-operatively) and/or medications to control blood pressure. Of course they have to take antibiotics prophylactically, as do other children with severe, congenital heart defects.
The biventricular repair is only available for a small subset of HLHS infants whose left ventricle is small, but not too small. The biventricular repair is actually a series of operations which must be performed in stages, like the Norwood Procedure; however, instead of converting the heart into a two-chamber pumping heart, the bi-ventricular repair encourages growth of the small left ventricle so that ultimately the child will have a fully functional, four-chamber pumping heart. Not as many facilities have experience performing this fairly new procedure, so some research on the part of the parents may be needed to find the ideal facility for their child.
Hypoplastic left heart syndrome occurs in up to four out of every 10,000 live births. It is one of the top three heart abnormalities to cause problems in the newborn. HLHS occurs slightly more often in boys than in girls.